Osteoarthritis
The disease of old age negatively impacts quality of life and eventual morbidity.
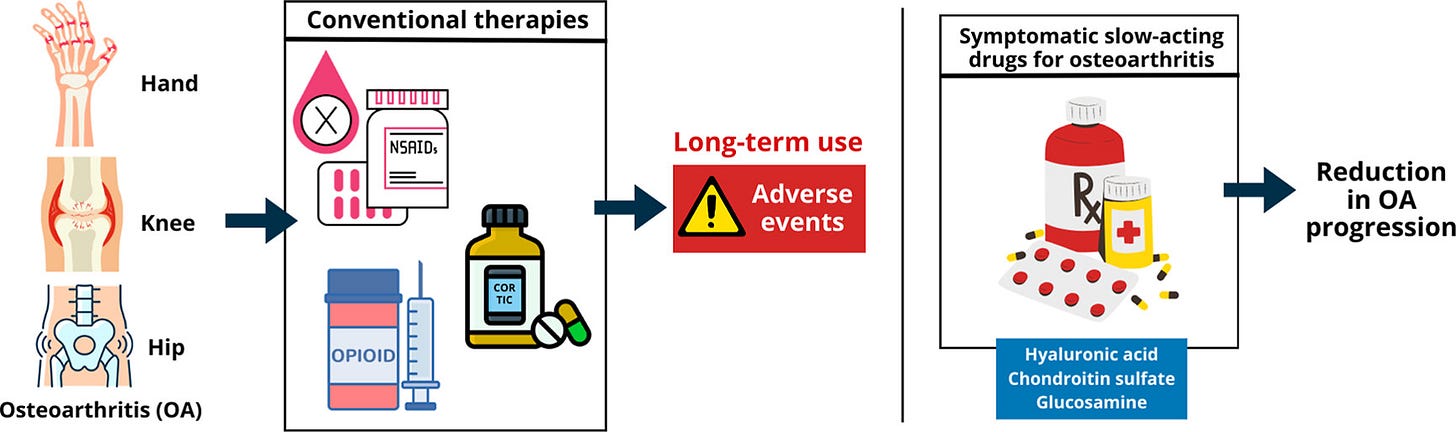
Osteoarthritis is a debilitating disease that increasingly affects older adults—especially as life expectancies increase. In 2017, it is estimated that more than 300 million people suffered from osteoarthritis worldwide (Shi). By 2021, that number had ballooned to nearly 600 million people (Silva). Alongside this debilitating disease, cardiovascular disease and diabetes mellitus are known to accompany it. While the effects of the disease on the individual lead to a diminished quality of life, the overall costs of this disease are absolutely staggering. However, there are known treatments. These treatment regimens include: NSAIDs (anti-inflammatory drugs like aspirin, ibuprofen, and naproxen), non-traditional NSAIDs (anti-inflammatory drugs like celecoxib, imrexcoxib, and etoricoxib), injections (intra-articular injections like hyaluronate), opioids (controlled substances like hydrocodone, tramadol, and hydromorphone), SYSADOAs (glucosamine and chondroitin), and physical therapy (building muscle).
Osteoarthritis is an inflammatory response. Moreover, inflammation occurs as a human body’s response to an injury. Namely, an injury will inflame and cause an injured area of the body to swell (allowing more blood to flow to the injured area). The increased blood flow will allow the body to attempt to heal the wound. The inflammatory response in osteoarthritis occurs when joint cartilage breaks down and the body attempts to repair—the joint will swell and be painful.
Moreover, there appears to be evidence that long-term use of opioids, NSAIDs, and corticosteroids leads to adverse reactions. More importantly, the safest route to addressing osteoarthritis is a combination of hyaluronates, glucosamine, and chondroitin sulfate. The researchers from Brazil cite that different kinds of hyaluronate produce various results. There are basically two types of hyaluronates: low molecular weight and high molecular weight. The researchers found that injecting both types (low molecular weight and high molecular weight) into osteoarthritic joints provided maximum benefits in the long run (Silva).
The use of chondroitin sulfate (although touted as a miracle drug in some circles) has been a steep climb for researchers. Some researchers report positive results while others report no positive results. However, pharmaceutical-grade chondroitin produced positive results.
The use of glucosamine proved to be positive, as well. It is a well-tolerated drug; however, it has been a steep climb for researchers to get a good handle on. In 2006, a highly cited study appeared in the New England Journal of Medicine, lending some credence to its efficacy. Moreover, the results were mixed—helping some patients and not others.
The major takeaway from this is that joint replacement surgeries (although not mentioned in the text above) are the best way to address extreme osteoarthritic symptoms. The use of the abovementioned therapies can delay surgery, but judicious care must be taken to strengthen muscle tissue surrounding impacted joints. The use of hyaluronic acid in conjunction with chondroitin and glucosamine can extend a person’s quality of life, but following your doctor’s orders is tantamount to extending your lifespan.
—
Sources and Footnotes;
Baden, Kyrie Eleyson R., et al. “The Safety and Efficacy of Glucosamine and/or Chondroitin in Humans: A Systematic Review.” Nutrients 17.13 (2025): 2093.
Clegg, Daniel O., et al. “Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis.” New England Journal of Medicine 354.8 (2006): 795-808.
De Roover, Astrid, et al. “Fundamentals of osteoarthritis: inflammatory mediators in osteoarthritis.” Osteoarthritis and Cartilage 31.10 (2023): 1303-1311.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: What is an inflammation? [Updated 2025 Apr 11].
https://www.ncbi.nlm.nih.gov/books/NBK279298/
Peck, Jacquelin, et al. “A comprehensive review of viscosupplementation in osteoarthritis of the knee.” Orthopedic Reviews 13.2 (2021): 25549.
Shi, J., Fan, K., Yan, L. et al. Cost Effectiveness of Pharmacological Management for Osteoarthritis: A Systematic Review. Appl Health Econ Health Policy 20, 351–370 (2022).
Silva, Vitor Alfredo de Santana, et al. “Impact of Symptomatic Slow-Acting Drugs on Inflammatory Pathways in Osteoarthritis: Therapeutic Advances and Future Challenges.” ACS Pharmacology & Translational Science 8.12 (2025): 4214-4236.


